Pronation Part I – What is pronation I
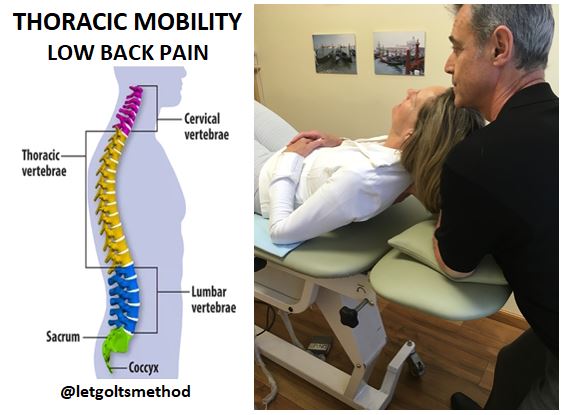
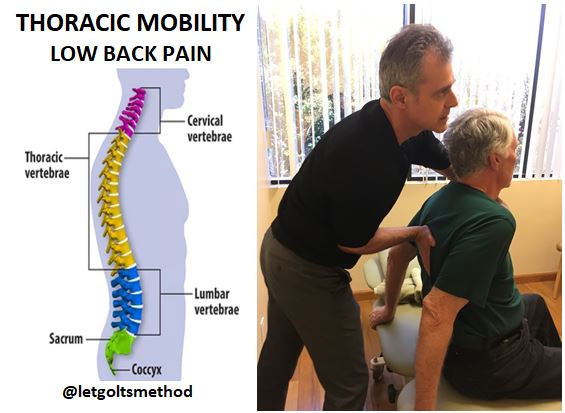
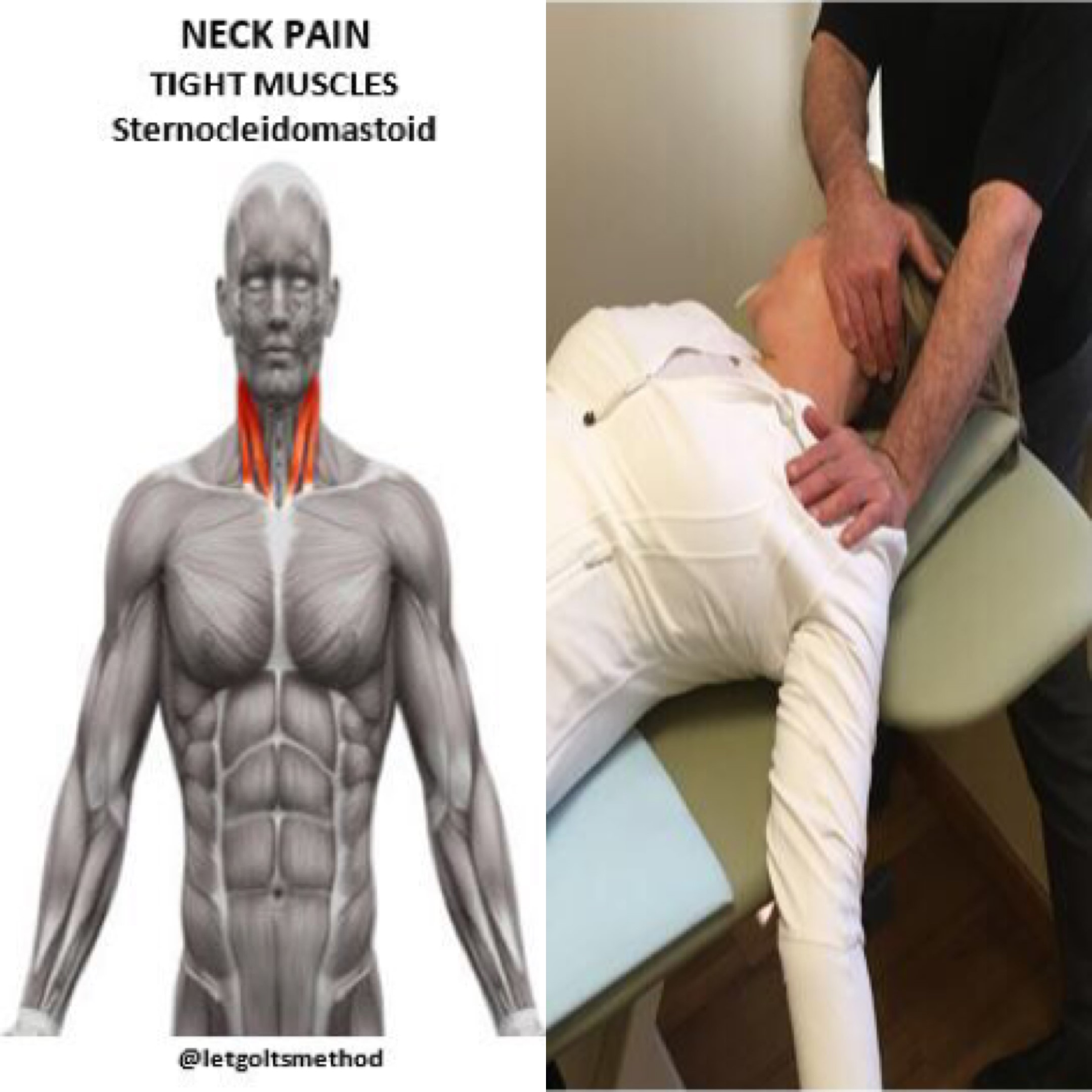
Up till now, our posts have addressed stiff upper backs, tight muscles, and certain postures that can contribute to chronic neck and/or low back pain. However, what we haven’t addressed is WHY the thoracic spine gets stiff and WHY those muscles get tight. More specifically, what causes them to end up that way and what causes your body to end up in the same position time and time again.
The answer? YOUR FEET! More specifically, pronation: the inward rotation of the foot when weight bearing. This forces the weight onto the inside of the foot, as opposed to being evenly spread when the foot is in a subtalar neutral (stable) position, as seen in below:
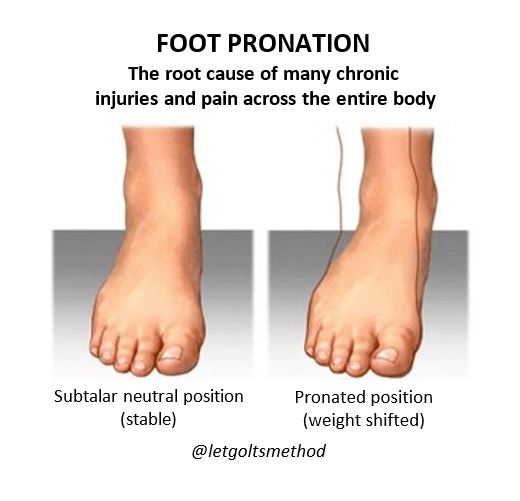
Pronating also often comes with a flattening of the arches, which shouldn’t be confused with flat feet (to be covered later on). As the foot pronates, the knee rotates internally, (represented in the video links below).
Pronation 1_3_pronation anterior view
Pronation 1_4_pronation posterior view
When this happens on both sides of the body, the hips will drop into anterior pelvic tilt. Once that happens, the body’s weight will begin to shift forward. In order to keep ourselves from falling forward, the lower back will extend backwards to maintain the center of gravity. In order to keep the center of gravity in line with the hips, the thoracic spine becomes curved while the shoulders round out. More often than not, the head will also be shifted slightly forward (“turtleneck” position).
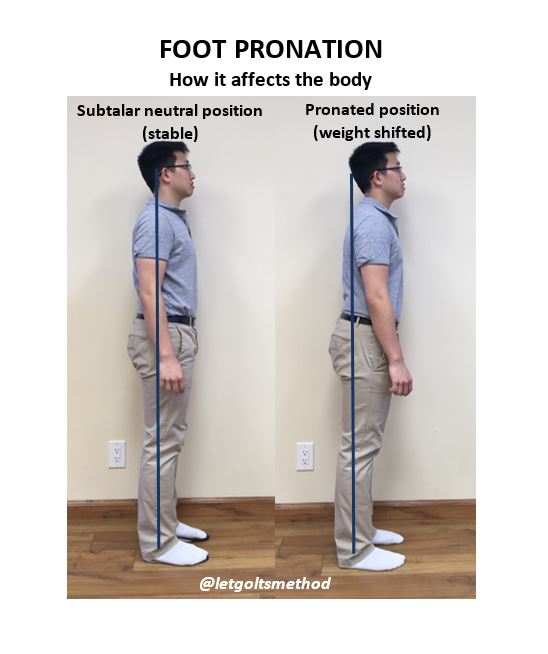
Here you can see how the body’s posture is affected by pronated feet vs feet set in subtalar neutral. The posture caused by pronation worsens over time as joints become stiffer and muscles become tighter. This chronic posture is why many people find it hard to simply sit or stand up “straight” and maintain that posture, as well as why many lower extremity injuries persist. It has nothing to do with how strong or weak the muscles are, but rather, with how their body compensates as a result of its structure – i.e., the bone structure of the foot having a bottom-up effect on areas higher up on the body.
 Los Angeles Magazine’s Best Physical Therapy Practice in LA
Los Angeles Magazine’s Best Physical Therapy Practice in LA